PAGE
Safety Guidelines for Hallucinogens - Research Excerpts
Contents
“Human hallucinogen research: guidelines for safety”
Annotated by TripSafe for faster reading
Johnson, M., Richards, W., & Griffiths, R. (2008). Human hallucinogen research: Guidelines for safety. Journal of Psychopharmacology, 22(6), 603–620. doi:10.1177⁄0269881108093587
The full paper is online here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056407/
These excerpts are designed to include pretty much everything that could be relevant to a non-clinical guide or participant, with headers/signposts to make reading easier. I find that reading scientific papers can be much slower than reading text with smaller sections and more headings.
Background
Why care?
Persisting adverse reactions are rare when research is conducted along these guidelines. Incautious research may jeopardize participant safety and future research. However, carefully conducted research may inform the treatment of psychiatric disorders, and may lead to advances in basic science.
Ayahuasca religious freedom act USA
Because the United States Supreme Court has recently ruled in favour of the União do Vegetal (UDV; a syncretic Brazilian church that uses ayahuasca in the context of religious ceremonies) in their claim that the UDV’s use of ayahuasca is protected under the Religious Freedom Restoration Act (Gonzales v. O Centro Espirita Beneficiente União do Vegetal, 2006), ayahuasca use within this church setting may receive increased scientific investigation within the USA.
Why say hallucinogen vs psychedelic
We use the word ‘hallucinogen’ herein to refer to the classical hallucinogens, sometimes called ‘psychedelics’, ‘psychotomimetics’ or ‘entheogens’ (Grinspoon and Bakalar, 1979; Ruck, et al., 1979; Ott, 1996; Metzner, 2004). Admittedly, the term ‘hallucinogen’ is not ideal for these substances, because perceptual changes are only one domain of their effects, and the typical perceptual changes engendered by hallucinogens at typical doses rarely include frank hallucinations (Grinspoon and Bakalar, 1979; Nichols, 2004; O’Brien, 2006). However, we use this term because it is the most widely used in the scientific literature. Although the term ‘psychedelic’ is widely used, it has the disadvantage of carrying considerable cultural connotation (i.e. its use as a descriptor of a style of music or art associated with Western counter-culture of the 1960s). The terms ‘psychotomimetic’ (emphasizing model psychosis) and ‘entheogen’ (emphasizing mystical-type experiences, i.e. phenomenologically indistinguishable from classically described mystical experiences) highlight only a single aspect (which may not occur reliably) of the much broader range of hallucinogen effects.
Purpose of the paper
The purpose of this paper is to provide guidance in the safe administration of high doses of hallucinogens (e.g. ≥25mg psilocybin or 200 μg LSD).
Lower doses
Some aspects of these recommendations may also apply to studies employing lower doses, although, as with other drug classes, the likelihood of potential adverse effects will be related to dose.
History of hallucinogen use by indigenous cultures
Hallucinogens have been used by indigenous cultures for millennia (Schultes, 1969; Lowy, 1971; Schultes, et al., 2001).
Remarkably, apparently without exception, such cultures view hallucinogenic plants and fungi as being of divine origin (Schultes, et al., 2001). Given this orientation, it is not surprising that their ingestion is often tightly restricted, with use controlled by ceremonial guidelines, including taboos against improper use (Schultes, et al., 2001; Weil, 2004).
Indeed, some of the safeguards developed for clinical hallucinogen research and expressed in the guidelines presented herein are similar to important aspects of hallucinogen use by indigenous cultures. These common themes are structured use (expressed as ritual in indigenous use), restrictions on use including the need for guidance and appreciation of hallucinogens’ powerful psychological effects (expressed as reverence in indigenous use).
Be careful of backlash
The growing controversy and sensationalism resulted in increasing restrictions on access to hallucinogens throughout the 1960s (ultimately resulting in the placement of the most popular hallucinogens into Schedule I of the 1970 Controlled Substances Act in the United States), creating substantially greater regulatory barriers for researchers to conduct human trials. The negative publicity also resulted in withdrawal of federal research funds, which had previously supported much of the human research, and in the professional marginalization of clinical investigators interested in pursuing research with hallucinogens.
Physiological safety
Hallucinogens generally possess relatively low physiological toxicity, and have not been shown to result in organ damage or neuropsychological deficits (Strassman, 1984; Gable, 1993, 2004; Halpern and Pope, 1999; Hasler, et al., 2004; Nichols, 2004; Halpern, et al., 2005). Nonhuman animal studies have shown MDMA (structurally similar to some classical hallucinogens, but with a substantially different pharmacological mechanism of action) to have neurotoxic effects at high doses, although MDMA has been judged to be safe for human administration in the context of several therapeutic and basic human research studies. In contrast, there is no evidence of such potential neurotoxic effects with the prototypical classical hallucinogens (i.e. LSD, mescaline and psilocybin).
Psychosis
In a survey of investigators who had administered LSD or mescaline, Cohen (1960) reported that only a single case of a psychotic reaction lasting more than 48 h occurred in 1200 experimental (non-patient) research participants (a rate of 0.8 per 1000). Notably, the individual was an identical twin of a schizophrenic patient and thus would have been excluded under the proposed guidelines.
The volunteer selection guidelines, addressed in a later section, will be the key factor in minimizing the risk of prolonged psychosis in human hallucinogen research studies.
Guidelines for safety
Although particular aspects of the proposed guidelines may be debatable, it is hoped that this paper will encourage such discussion while conveying the general themes and major domains of concern in human hallucinogen research. The proposed guidelines may serve as a helpful starting point for investigators planning to conduct human hallucinogen research.
Selection of volunteers
Generally healthy
In our studies at Johns Hopkins, participants must be in good general health as assessed by detailed medical history, physical examination, 12-lead ECG, blood chemistry profile, haematology and urinalysis. Pregnant women or those not practicing effective means of birth control are excluded.
Blood pressure
Relevant to general medical screening, classical hallucinogens moderately increase pulse and both systolic and diastolic blood pressure (Isbell, 1959; Wolbach, et al., 1962b; Strassman and Qualls, 1994; Gouzoulis-Mayfrank, et al., 1999; Passie, et al., 2000; Griffiths, et al., 2006). Therefore in our studies of psilocybin to date, volunteers have been excluded if resting blood pressure exceeded 140 systolic and 90 diastolic (mmHg), averaged across four assessments on at least two separate days.
Medication exclusions
Specifically, chronic administration of tricyclic antidepressants and lithium (Bonson and Murphy, 1996), and acute administration of serotonin reuptake inhibitors (Fiorella, et al., 1996) and the antipsychotic medication haloperidol (Vollenweider, et al., 1998) have been shown to potentiate hallucinogen effects, and therefore participants’ use of these represents a safety concern. Chronic administration of serotonin reuptake inhibitors (Stolz, et al., 1983; Strassman, 1992; Bonson, et al., 1996) and monoamine oxidase inhibitors (Bonson and Murphy, 1996) have been shown to decrease sensitivity to hallucinogens, and therefore participants’ use of these represents a scientific concern.
It should also be noted that administration of ayahuasca (which contains monoamine oxidase inhibitors in addition to DMT) to individuals taking serotonin reuptake inhibitors may lead to a severe serotonin syndrome reaction (Callaway and Grob, 1998).
Supplement exclusions
We also advise investigators to include questions concerning over-the-counter dietary supplements in addition to prescription medications when probing medication history, and to exclude those taking potentially problematic substances (e.g. 5-hydroxytryptophan and St John’s Wort may affect serotonergic function, and, therefore, it is appropriate to exclude individuals currently or recently taking these products).
Psychiatric screening
Thorough psychiatric interviews (e.g. SCID; First, et al., 2001) should be conducted to identify contraindicated psychological functioning or history. In our research, individuals are excluded who have a current or past history of meeting DSM-IV criteria for schizophrenia or other psychotic disorders (unless substance-induced or due to a medical condition), or bipolar I or II disorder, which are the most important conditions to exclude for ensuring safety. We also exclude those with a first or second-degree relative with these disorders.
Rigidity and emotional lability (Emotional lability is a disorder characterized by involuntary emotional displays of mood that are overly frequent and excessive, often the result of various neuropathologies) personality traits
Other investigators have also excluded individuals scoring high on the personality traits of rigidity and emotional lability on the grounds that these have been significantly associated with negative experiences during hallucinogen action and during non-pharmacologically induced altered states of consciousness (Dittrich, 1993; Hasler, et al., 2004).
More psychiatric disorders
This strategy is warranted because the effects of hallucinogens may potentially interact with various psychiatric disorders. Furthermore, including volunteers with psychiatric disorders may increase the chances that symptoms from such disorders may inadvertently be misattributed to hallucinogen action. For example, our recent studies with healthy volunteers have excluded volunteers with a current or a recent past history (e.g. within the last 5 years) of alcohol or drug dependence (excluding caffeine and nicotine) or major depression, and volunteers with current obsessive-compulsive disorder, dysthymic disorder, panic disorder, dissociative disorder, anorexia nervosa or bulimia nervosa.
Study personnel / trip sitters
Importance of good sitters / monitors
It is difficult to overemphasize the importance of the interpersonal atmosphere created by study staff in influencing a volunteer’s response to a hallucinogen. Most critically, this applies to the interpersonal environment created by the actual session monitors (Leary, et al., 1964; Masters and Houston, 1966).
Qualities of good sitters / monitors
The monitors should be knowledgeable about the medical and psychological markers of potential adverse reactions to the drug. Furthermore, monitors should have significant human relation skills and be familiar with descriptions of altered states of consciousness induced by hallucinogens. Personal experience with techniques such as meditation, yoga or breathing exercises may also prove to be helpful in facilitating empathy for volunteers who experience altered states of consciousness during hallucinogen action. The lead monitor for each participant in the Johns Hopkins studies to date has been a clinical psychologist or a clinical social worker. However, we believe that clinical sensitivity (e.g. empathy, respect) is likely more important than formal degrees when considering monitor qualifications.
Two monitors is best
We recommend the presence of at least two monitors during hallucinogen administration sessions so that the volunteer will never be alone should one monitor need to briefly leave the session room (e.g. to the restroom). For each participant in the Johns Hopkins studies, we have specified a primary monitor (who takes the lead in participant interactions) and an assistant monitor, with differing required levels of involvement for the two monitors during volunteer preparation (see Preparation of volunteers section below).
Monitor gender
In prior research into potential treatment applications of hallucinogens, the presence of both genders in the monitoring team has been recommended (Grof and Halifax, 1977; Grof, 1980; Kurland, 1985). Having both genders present may foster feelings of security. In the Johns Hopkins studies, we have followed this recommendation when possible, but also have conducted sessions in which the primary and assistant monitors were of the same gender as the volunteer. We would counsel against both members of the monitoring team being the opposite gender of a volunteer, unless there is a staff member of volunteer’s gender who has established some rapport with the volunteer in advance, and who can quickly be summoned to assist should support be needed in the restroom.
Importance of all people around
all individuals at the study site having contact with the volunteer on or before the session day may influence a volunteer’s reaction to a hallucinogen. Pre-session negative mood consisting of anxiety or depression has been shown to significantly predict anxious or other negative experiences during the session (Metzner, et al., 1965).
Good qualities of people
friendly, welcoming and compassionate
The staff member should maintain a positive social rapport with the volunteer to reduce the likelihood of adverse psychological reactions during the session and to gain accurate information on the volunteer’s condition so that other study staff may be notified if there is any potential reason to postpone or cancel the session
Physical environment
Pleasing environment
First, an aesthetically pleasing environment may decrease the probability of acute psychological distress. The Johns Hopkins hallucinogen research projects use a living room-like setting (Figure 1). The furniture is comfortable and is atypical for a research laboratory or medical office setting. An overly ‘clinical’ environment with an ‘antiseptic’ look (e.g. white walls, extraneous medical equipment, personnel in white lab coats) may increase anxious reactions.
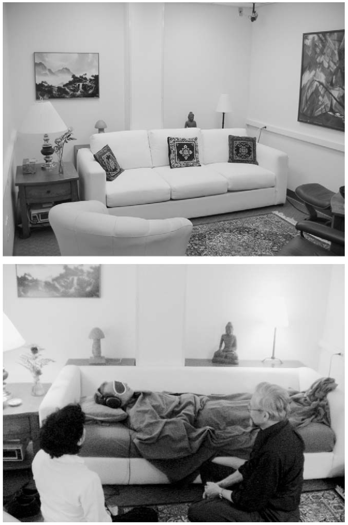
The living room-like session room used in the Johns Hopkins hallucinogen research studies. Aesthetically pleasing environments such as this, free of extraneous medical or research equipment, in combination with careful volunteer screening, volunteer preparation and interpersonal support from two or more trained monitors, may help to minimize the probability of acute psychological distress during hallucinogen studies. For studies that investigate potential therapeutic effects or the phenomenology of introspective hallucinogen experiences, the use of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel.
Safety of environment
The environment should be designed keeping in mind the perceptual changes and disorientation that can occur under the influence of hallucinogens. Thus, any potentially dangerous objects (e.g. furniture with sharp corners; glass lamps) should be avoided. If there is a window in the room, the investigators need to be confident that the volunteer could not exit the window if in a delusional state.
No phones
Additionally, the session room should not have a telephone, and the participant should surrender her or his cellular telephone before the session.
Preparation of volunteers
Volunteer consent
volunteer preparation at the earliest stages must include a thorough review of the consent form, which should include in plain language the range of experiences that may result from hallucinogen administration, including changes in perception, sense of time and space, and emotion (possibly including anxiety, fear, panic and paranoia). Relative to other drug classes, the subjective effects of hallucinogens are likely more difficult to describe to a naïve volunteer; therefore, additional time may be necessary to fully discuss these potential effects with volunteers. The consent form should also include the approximate timecourse of the drug, the state of knowledge concerning its toxicity profile, and its status as an experimental drug. In addition, the consent form should state that there is a relatively small risk of adverse effects that last for hours to days after the hallucinogen session. These include mood disorders (such as depression), psychotic disorders and anxiety disorders. It should also state that there are rare reports in which hallucinogen exposure appears to cause, accelerate or precipitate the onset of significant or lasting psychiatric illnesses such as psychoses and intermittent or persisting visual perceptual abnormalities (‘flashbacks’, HPPD).
Building rapport and trust
The next step in volunteer preparation is to conduct a series of meetings between the monitors and volunteer to build rapport and trust. The relationship between the monitors and the volunteers should be well established by the time of the first session (Masters and Houston, 1966). In the Johns Hopkins studies, there are at least eight contact hours over the course of at least four meetings, usually over a 1-month period. One of these preparatory meetings should be conducted in the room in which the hallucinogen is to be administered, to familiarize the participant with the physical environment. The primary monitor meets with the volunteer during all of these meetings, while the assistant monitor is required to be present on at least one occasion. It is important that the assistant monitor, in addition to the primary monitor, has developed a trusting relationship with the volunteer because this assistant monitor will be the only person in the session room with the volunteer if the primary monitor needs to leave briefly.
Content of preparatory meetings
During these preparatory meetings, the monitors discuss meaningful aspects of the volunteer’s life. The main purpose of the participant–monitor meetings is to develop rapport and trust, which we believe helps minimize the risk of fear or anxiety reactions during the hallucinogen session. This typically includes discussions of the volunteer’s childhood, romantic life, current relationships with family and friends, and the volunteer’s philosophical and/or spiritual beliefs. Reviewing personal history and feelings may be important for two reasons. First, this discussion helps establish a significant level of trust. The interaction should convey that all aspects of the person are welcome, from the petty to the noble, from embarrassments to achievements and from sorrow to joy. By the time of the hallucinogen session day, the volunteer will ideally feel completely comfortable with the monitors, reducing the likelihood of paranoia (e.g. feeling that the monitors are trying to control her or his mind, or have deceived the volunteer about the nature of the study). Second, related personal material may ‘emerge’ under the effects of the hallucinogen. That is, the volunteer may experience intense thoughts, feelings and visions related to his or her personal history or world-view. Knowing about the volunteer’s life will allow the monitors to better understand her or his session experience and help the monitors in providing interpersonal support should strong emotions arise. If it is felt that sufficient rapport and trust have not developed during these monitor meetings, then either additional contact hours should be provided, or the volunteer’s participation should be cancelled. A high dose of a hallucinogen should not be administered to a volunteer if sufficient trust has not been established.
Preparing volunteers on bodily effects
The preparation of the volunteer should involve a detailed discussion of the possible range of experiences that may be encountered after hallucinogen administration. This includes the typical onset and duration of the drug(s) under investigation. Preparation involves discussion of the various potential physical sensations, such as nausea or heightened awareness of physiological processes, such as breathing and heartbeat. Volunteers are encouraged to trust that their bodies will continue to function properly regardless of such sensations, and that these bodily processes will continue without the volunteers’ volitional control.
Preparing volunteers on psychological effects
The major categories of potential psychological experiences during hallucinogen action should be discussed with the participant. The range of subjective experience under hallucinogens can be remarkably broad (Blewett and Chwelos, 1959; Richards, 1980; Masters and Houston, 1966; Strassman, 2001; Nichols, 2004; Stolaroff, 2004). This range of experiences includes perceptual changes, such as visual illusions, intensification of colours, proprioceptive changes (e.g. one’s body may feel gigantic or tiny), and synesthesia (e.g. seeing sounds or hearing colours). Another type of possible experience is the alteration of emotions, such that emotions of either a positive or negative nature may be greatly intensified, yielding experiences that may range from euphoria to despair. Another category of possible effects involves changes in the sense of time and space. At the extremes, time and/or space may be experienced as infinite or nonexistent. Other experiences may include thoughts, feelings or insights concerning one’s personal history (e.g. revisiting childhood memories) or current life circumstances (e.g. relations with loved ones), highly symbolic experiences (e.g. involving religious symbols, animals, etc.), and experiences described by some to be of a mystical or spiritual nature. Importantly, it should be emphasized that these experiences may consist of much more than the participant subjectively observing internal and external events. Rather, the effects may involve a profound change in one’s sense of self, such that one feels as if he or she is merging into the surrounding environment or the entire universe (Schultes, et al., 2001). The individual may temporarily experience a complete loss of subjective self-identity, a phenomenon sometimes referred to as ‘ego loss’ or ‘ego death’ (e.g. Leary, et al., 1964; Grof and Halifax, 1977; Grof, 1980).
a detailed discussion concerning the range of possible hallucinogen effects will enhance safety by psychologically preparing the participant for the unique and often intense effects of a hallucinogen
Informing volunteers how to handle difficult experiences
The volunteers should be given guidance on how to handle difficult hallucinogen experiences. Whether the disturbance consists of frightening illusions or internal imagery, difficult thoughts and feelings about some past or present personal issue, or anxiety related to a radical change in sense of self (e.g. temporary loss of self-identity), the volunteer is encouraged to mentally surrender to the experience, trusting that her or his usual state of consciousness will return when the drug effects resolve (Blewett and Chwelos, 1959; Masters and Houston, 1966; McCabe, 1977). For example, if the participant experiences disturbing internal imagery of a demon or monster, he or she is encouraged to mentally approach the figure and interact with it (e.g. imagine asking the figure why it has appeared), rather than attempt to flee from the disturbing imagery. The participant should be alerted that sometimes people experience extremely convincing sensations of dissolving, melting, exploding and so forth, and that the best way to deal with all such situations is to surrender to the experience, subjectively allowing oneself to dissolve, melt or explode. Similar advice applies to physical symptoms such as nausea; for example, participants may be encouraged to ‘dive in’ to their stomachs, which may alleviate the nausea, as it has been suggested anecdotally that nausea and other somatic discomforts may in part be of a psychosomatic nature (Blewett and Chwelos, 1959; Masters and Houston, 1966).
Not encouraging them to read about typical experiences
In the Johns Hopkins studies, we have not encouraged participants to read the diverse and widely varying published accounts of hallucinogen effects as part of their preparation, because this may introduce compelling idiosyncratic expectations.
During the session / trip
Blood pressure
Furthermore, medication for the treatment of acute hypertension (e.g. intravenous labetalol) should be immediately available in the event that blood pressure exceeds predetermined safety parameters.
Restroom visits
If the volunteer needs to walk to complete study tasks or to go to the rest room, the monitors should stand close by to assist by gently holding an arm or shoulder. Even with high doses of hallucinogens, individuals do not typically show substantial motor impairment, and will likely be able to ambulate without considerable difficulty (with the exception of hallucinogens such as parenteral DMT with abrupt effects and short duration of action). However, perceptual and proprioceptive effects may make walking disorienting, which is why gentle guidance may be helpful.
Either the restroom door needs to have no lock, or study staff should have a key readily available if needed.
Don’t leave them alone
One of the monitors should always be present in the session room with the participant.
Don’t have other people interact with them
Because the session monitors will have developed rapport and trust with the participant, they should be the only people to interact with the volunteer during the course of hallucinogen action, barring any non-routine event (e.g. fire alarm, medical intervention by a specialist). Individuals who are anticipated to have contact with the volunteer during the course of hallucinogen action (e.g. nurse, physician) should have at least met with the volunteer once prior to session to develop some degree of rapport and trust.
If they try and leave
Any attempt by a disoriented volunteer to leave the session area would be met with compassionate but firm direction to return to the session room.
Interestingly, the volunteer who fled Strassman’s (2001) study site on psilocybin was a carefully screened, experienced LSD user. Therefore, it is imperative for safety reasons that the study site environment, session procedures and participant preparation all minimize the chance of a volunteer leaving the study site.
Unexpected scenario
On the single occasion at Johns Hopkins in which a fire alarm sounded during a session, the two study monitors closely escorted the volunteer outside, making sure to minimize contact with other individuals. The three of them walked to a nearby quiet area with an attractive landscape and enjoyed the scenery until the volunteer and monitors could return to the building. The monitors encouraged the participant to view the occasion as an opportunity to enjoy the natural world outdoors (something normally unavailable during sessions), rather than as an impediment to having a successful session. If any non-routine events occur, the monitors should maintain contact with the volunteer throughout.
If they become anxious
If participants become anxious during the course of hallucinogen action, it is now widely recognized that the appropriate first response is to provide strong personal support and reassurance (O’Brien, 2006). This primarily includes interacting with the volunteer in a comforting and reassuring manner. If the volunteer is behaving anxiously and a negative psychological reaction seems to be escalating, the monitors should convey a solid sense of security and calm, while empathizing with what may be an incredibly intense and unpleasant experience. Attempts to ‘talk down’ the participant (i.e. the use of reality-defining techniques to distract the participant from or attenuate the altered state of consciousness) may be counterproductive and aggravate a difficult reaction (McCabe, 1977). Instead, participants should be reminded to surrender to the experience. Appropriate forms of reassurance may include a supportive touch to the arm or shoulder with verbal reminders that the participant is in a research study, has taken the hallucinogen, and that he or she will return to normal consciousness in ‘a few minutes’ or ‘a few hours’ (or whatever the appropriate estimate may be, depending on the specific drug under study and when it was administered). During an intense hallucinogen-occasioned experience when verbal interactions may be of limited help, a powerful form of reassurance (sometimes called ‘interpersonal grounding’) is simply holding the hand of the participant (McCabe, 1977). Many volunteers report that during such experiences, a reassuring hand provides an incredible sense of stability and connection. Monitors should demonstrate this practice during preparation to normalize hand holding during sessions.
Will this be enough to deal with difficult experiences?
If volunteers have been appropriately screened and the guidelines herein followed, reassurance should be sufficient to diffuse acute psychological distress in the vast majority of cases. For example, in recent studies in our laboratory, in which we have administered high doses of psilocybin to 54 volunteers, reassurance has been sufficient to handle all cases of acute psychological distress that have arisen.
If distress can’t be managed with reassurance alone: 10mg Valium (diazepam), Xanax is less preferable as it takes longer to onset [1], but if used 0.5mg Xanax is equivalent in effect to 10mg Valium [2]
For cases in which acute psychological distress is insufficiently managed with reassurance alone, treatment with a benzodiazepine anxiolytic is the pharmacological intervention of choice (Abraham and Aldridge, 1993; Frecska and Luna, 2006; O’Brien, 2006). In these cases, we recommend a 10 mg oral dose of diazepam (Grinspoon and Bakalar, 1979), although oral doses of 15–30 mg per hour or every few hours as needed have been recommended for pharmacological treatment of ‘bad trips’ that do not respond to reassurance in emergency department settings (Ungerleider and Frank, 1976). Because of its high lipid solubility, diazepam has a more rapid onset, a shorter time until peak plasma concentration and a shorter duration of therapeutic action than many other benzodiazepines including lorazepam, despite the fact that lorazepam has a shorter elimination half-life (Greenblatt and Shader, 1985; Funderburk, etal., 1988). Although the intravenous route may be considered, the oral route is preferable because intravenous injection procedures may further exacerbate the participant’s anxiety.
Anti-psychotics
Moreover, antipsychotic medications (e.g. risperidone, olanzapine) should be available in the event that an adverse reaction escalates to unmanageable psychosis. However, experienced clinicians have suggested that although antipsychotic medications may reduce psychotic behaviour through sedation, their use may be problematic because the effects may be abrupt, unpleasant and intense and their use may result in subsequent psychological problems (McCabe, 1977; Grinspoon and Bakalar, 1979; Grof, 1980). Furthermore, pretreatment with the antipsychotic haloperidol has been shown to exacerbate the psychosis-like effects of psilocybin (Vollenweider, et al., 1998), suggesting that haloperidol should not be used as a rescue medication. Although not approved for use in the USA, ketanserin (a 5-HT2A antagonist) pretreatment has been shown to attenuate psilocybin effects (Vollenweider, et al., 1998), suggesting possible use as a rescue medication for hallucinogen administration.
Emergency room
Bringing the participant to the emergency department represents an ultimate ‘last resort’ in the treatment of a very difficult (i.e. psychotic) reaction. However, medical evaluation by well-meaning emergency department personnel, who are inexperienced with hallucinogen effects can readily escalate and prolong an adverse reaction. Therefore, all possible efforts should be made to treat a difficult experience in the session context, even if pharmacological intervention is required.
Checking-in
In studies such as ours, in which participants are encouraged to focus their attention inward by wearing eyeshades and listening to music through headphones, our advice is for monitors to occasionally probe the volunteer’s psychological well-being (e.g. ask the volunteer, ‘Would you like to describe where you find yourself?’) to ensure that the volunteer is not experiencing significant anxiety and is in need of support.
Q to figure out: What defines occasionally?
Eyeshades and headphones
the employment of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel. This may be especially important for volunteers who are experiencing the effects of a hallucinogen for the first time. Typically, we have kept eyeshades and headphones in place for most of the session. In the latter hours of the session some time is spent with the volunteer sitting on the couch, interacting without eyeshades and headphones, although music may still be played through speakers to provide nonverbal structure and continuity.
Discussing while tripping?
As a whole, we encourage our participants to ‘collect experiences’ to discuss after the drug effects have abated, and discourage attempts to analyse material or communicate excessively while the atypical states of consciousness are still occurring.
No driving for the remainder of the day
Ability to contact the monitor
We have also given the participant the primary monitor’s pager number to call if he or she feels the need for support that evening. Of the 54 volunteers tested at a high psilocybin dose to date, no one has paged the monitor, although volunteers do seem to appreciate this opportunity for additional support.
Post-session
After the session, safety monitoring should continue in the form of one or more post-session meetings (typically the next day) between the primary monitor and participant to ensure psychological stability and provide an opportunity for the volunteer to discuss thoughts or feelings from the session.
A person to discuss with
As with any acute, intense positive or negative emotional experience, participants often feel the need for, and seem to benefit from, additional time for reflecting on the novel thoughts and feelings that may have arisen in the session. Given the potentially intense and unusual psychological nature of hallucinogen effects, the volunteer may have difficulty discussing the experience with others in her or his life. Because the monitors were present during the session when the hallucinogen effects were experienced and have knowledge of a broad range of reported phenomena during drug action, the volunteer may feel more comfortable discussing her or his experience with the monitors than with others.
Acknowledgements
Support for preparation of this manuscript was provided by grants from NIH (R01 DA03889), the Council on Spiritual Practices and the Heffter Research Institute. We thank George Greer, MD, Charles Grob, MD, Robert Jesse, Annie Umbricht, MD and Franz Vollenweider, MD for helpful comments on previous versions of this manuscript. We also thank the staff of the Johns Hopkins psilocybin research studies, whose insights have contributed to these guidelines, including Mary P. Cosimano, MSW and Brian D. Richards, Psy.D. for their roles in screening volunteers and monitoring sessions, and Lawrence P. Carter, PhD, Ryan K. Lanier, PhD, Benjamin McKay, Chad J. Reissig, PhD, and Ryan G. Vandrey, PhD for their assistance in monitoring sessions.
- 15 More Pages
- Psychedelic Psychotherapy: A Strong Endorsement
- The Best Books About Psychedelic Therapy
- Are dabs bad for you?
- How Long Do Shrooms Last?
- Psychedelic Addiction: Treatment
- Study suggests psychedelic drugs increase people's sense of connectedness - to the self, others, and the world
- First Time LSD User? Read this.
- How to Have a Good Shroom Trip
- LSD Test Kits
- How to avoid a bad trip
- An Acid Trip: What is an acid/LSD trip like?
- How long does it take for acid to kick in?
- LSD vs Acid
- What is LSD?
- Safety Guidelines for Hallucinogens - Research Excerpts
- Disclaimer
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Have more questions, or want more resources and info? Visit /r/PsychedelicTherapy or /r/Psychedelics.